Evaluation of Community-based EoLC programmes

Beneficiaries
The EoLC programmes delivered by four NGOs had benefited altogether 2,392 community-dwelling patients and their family caregivers over the three years. Regarding home-based EoLC services, altogether 777 patients and their family caregivers were served between 2016 and 2018. These patients comprised of 50.7% cancer patients, 18.5% with renal disease, 13% with COPD, and the remaining consists of patients with various non-cancer conditions.
Methodology
To evaluate the outcomes and impacts of the community-base EoLC programmes, a common evaluation framework was developed. Patients and their primary family caregivers were assessed by pre-post-follow up clinical assessment using standardised measurements. For patients, their physical symptoms, depression, anxiety, and practical concerns were assessed by “The Integrated Palliative Care Outcome Scale” (IPOS) at service intake, one month after service, and three months after the service respectively. For family caregivers, their stress around caregiving was assessed by the “Caregiver Strain Inventory” (CSI) at service intake and three months after the service respectively. Level of grief was assessed by the Chinese “Inventory of Complicated Grief” (ICG) at two months after the patient’s death. Apart from clinical assessment, patients and family caregivers were also surveyed for their satisfaction towards services by the research team from the University of Hong Kong.
Regarding service impact, the medical service utilisation in the last 6 months in life of deceased patients in the community-based EoLC programme was compared to that of deceased end-of-life patients in 2015 in Hong Kong who had a principal diagnosis of cancer, COPD, congestive heart failure, end-stage renal diseases, motor neuron disease, and Parkinson’s disease. These data were retrieved from the Central Panel on Administrative Assessment of External Data (CPAA) of Hospital Authority in a clinical data mining (CDM). With the introduction of EoLC services, it is expected that there would be an impact on the medical service utilisation of patients in the last few months in life.
In addition, a survey was conducted with “community partners” of the five JCECC EoLC programmes between March and April in 2018. These “community partners” include service agencies, hopsitals, RCHEs and CGATs which have referred clients to the community-based or RCHE EoLC programmes under JCECC Project. This survey aims at exploring the satisfaction level and views of these “community partners” regarding the overall contribution and effectiveness of the JCECC EoLC services.158 completed questionnaires were received after sending out 224 of invitations. The response rate was 70.54%.
Achievements
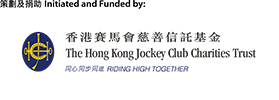
Patients reported significantly improved quality of life:
- Among assessed patients (n=283), after 3 months of service, they reported 18% reduction of physical symptoms, 47% and 31% reduction in depression and anxiety respectively, and the reported practical concerns reduced by 55% when compared to service intake. All these changes were statistically significant (p<.001).
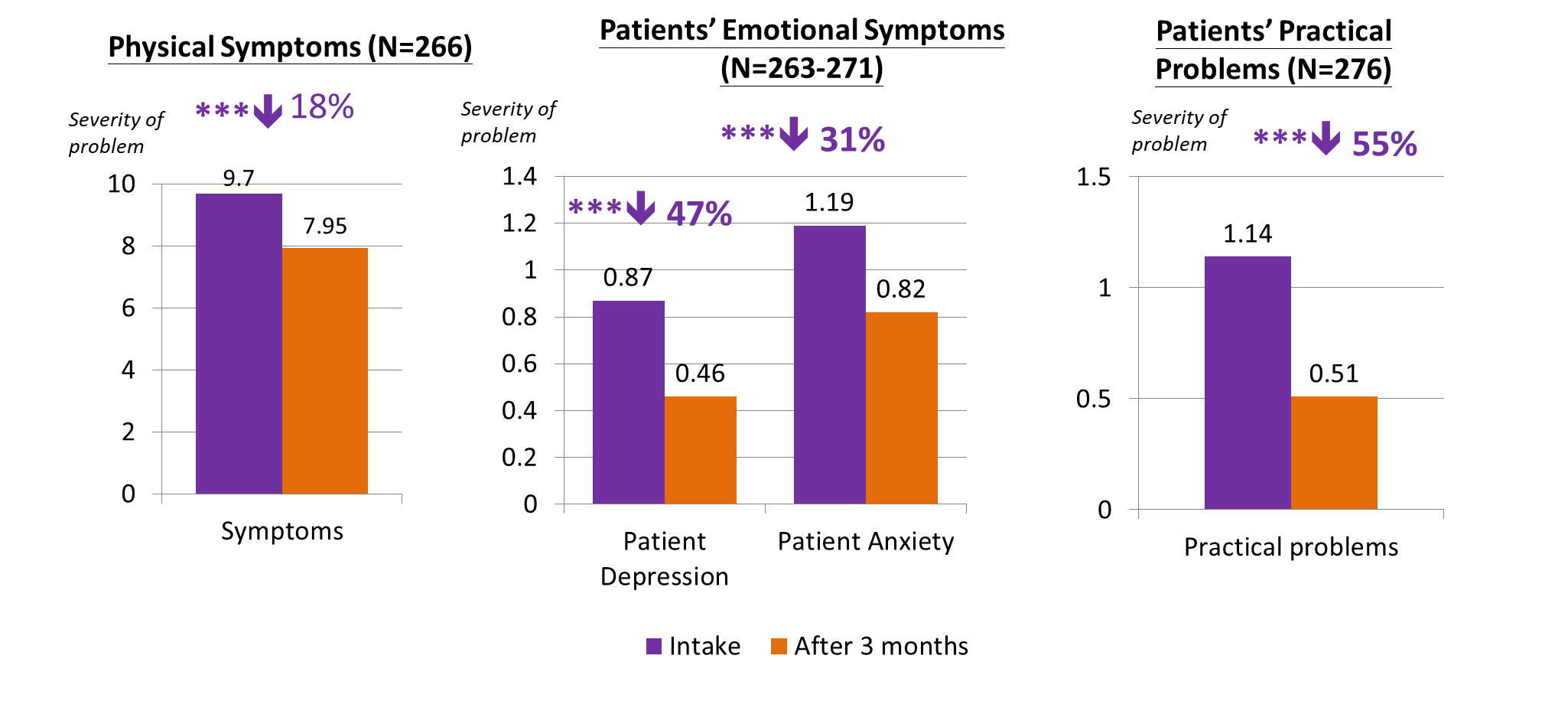
Family caregivers reported significant improvements in caregiving stress and emotions:
- After 3 months of service, family caregivers (n=164) reported 19% reduction in caregiver strain and 27% reduction in anxiety. These changes were statistically significant (p<.001). Moreover, almost 90% of the assessed bereaved family caregivers (n=166) reported low level of complicated grief two months after the patient’s death.
Reduced unnecessary medical service utilisation
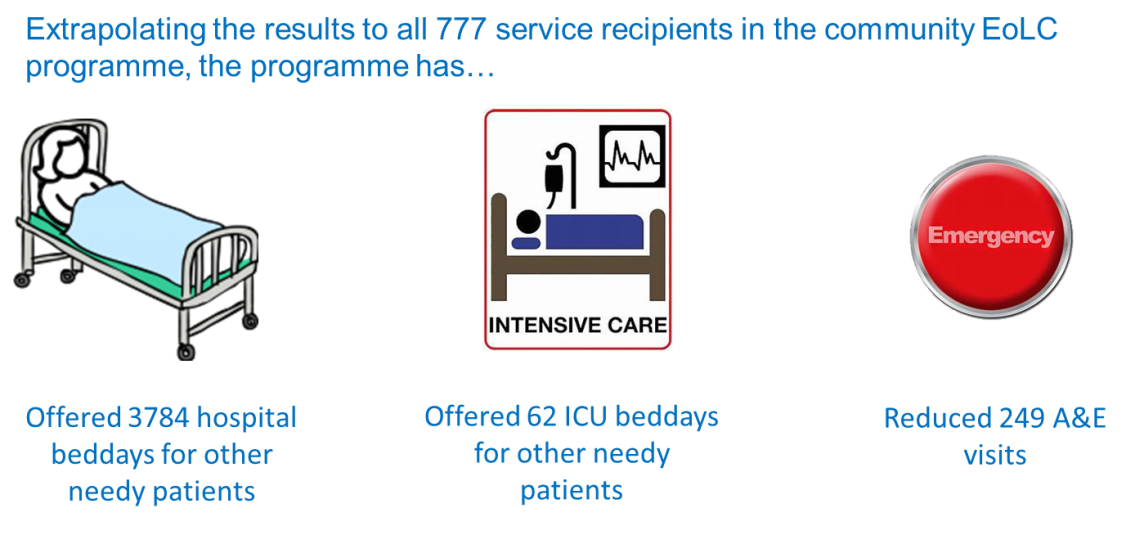
- Regarding service impact on medical service utilisation in the last 6 months of life, retrievable data from 221 deceased patients suggested that the programme patients had 4.87 fewer hospital beddays and 0.32 fewer A&E attendances, and 0.08 ICU beddays fewer than EoL patients in general. This result supports the effectiveness of the community-based EoLC programmes in helping patients to avoid unnecessary hospitalisation and stay home longer.

- Projecting this finding to 777 patients served by the four NGOs, the programme would have helped spared 3,784 hospital bed days, 162 ICU beddays, and 249 A&E attendance to other needy patients. Taking the cost of these medical service into consideration, the programmes have also helped save 20.6 million medical costs.
High service satisfaction
- Majority of the surveyed patients and family caregivers reported highly satisfied experience with the services. Among the surveyed patients (n=120) and family caregivers (n=148), 95.7% and 94.6% respectively express high level of overall satisfaction towards the services.
- Not only patients and family caregivers, the survey with “community partners” revealed that majority (89%) of the agencies that referred cases to or work with the JCECC EoLC service teams were highly satisfied with the collaboration experience. Overall, 90% were highly satisfied with the EoLC programme, and 89.8% would recommend this service to other organisations. Furthermore, 91% and 89% strongly agreed that “the EoLC programme brought positive changes to the service of the organisation of the referrers”, and that “the programme brought positive changes to worker’s relationship with patients” respectively.
Learnings in phase I and way forward in phase II
- The community-based EoLC programmes were effective in promoting quality of life of both patients and their family caregivers. Moreover, it showed promising effectiveness in reducing unnecessary medical service utilisation among patients. The services also provided highly satisfying experience for most patients and family caregivers. Not only patients and family caregivers, collaborating community partners that refer cases to the EoLC programmes also expressed high level of satisfaction towards the programme. More importantly, the responses reflected that the services promoted communication between patients and family members with the community partners, which have implications on the continuity and coordination of care across care settings, and thus satisfaction of patients and caregivers towards the overall care experience in the community.
- Based on the findings from the first 3 years, effective service components in the 4 community-based EoLC models were identified and further streamlined to develop a unified service model which could be replicated and serve as reference service model for other EoLC in Hong Kong – the Integrated Community End-of-Life Support Team (ICEST).